The long-suspected role of the importance of immunity in cancer has gained strong experimental support in the past decade. Infiltrating immune cells can function to control tumor growth or to help create an immunosuppressive environment in which the tumor can thrive. Immune surveillance by T-cells in human cancers is one of the key mechanisms of anti-cancer immunity.
For colorectal cancer, an “immunoscore” based on the quantification of two types of T-cells (CD3+ and CD8+) in the tumor center and in the advancing tumor margin has turned out to be the best prognostic predictor for survival. Also for hepatocellular carcinoma similar immunoscores have been devised but the outcome has been less convincing.
The CD3 complex is required for the surface expression of T-cell receptor and for intracellular signaling. Engagement of the T-cell receptor–CD3 complex by antigenic epitopes in the context of MHC-molecules subsequently initiates proliferation and differentiation of the naive T cell into T-effectors. The CD3 is membrane-bound antigen of all mature T-cells, and it is virtually not expressed by other cell types. This high specificity makes it a useful immunohistochemical marker for T-cells in tissue sections. CD3 is also an excellent marker because of the quality of the staining and the stability of this antigen.
We are working now on identification and quantification of CD3+ T-cells in several regions of interest (Fig.1) within tumor and non-tumor liver tissue in patients with hepatocellular carcinoma.
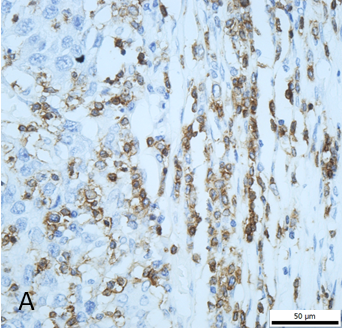

Figure 1. Results of immunohistochemical staining for CD3+ T cells. A, CD3+ cells at the invasive margin of hepatocellular carcinoma (400×). B, regions of interest (100×): tumor center (TC), tumor invasive margin (TIM), and non-tumor parenchyma (NT), dotted line: tumor border, the area between the dashed lines: tumor invasive margin.